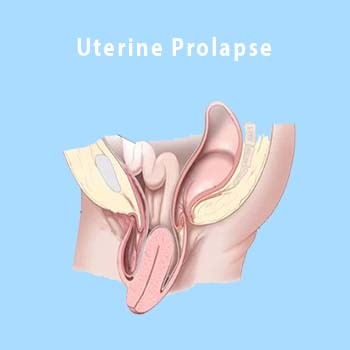
UTERINE PROLAPSE
-
Uterine prolapse occurs when pelvic floor muscles and ligaments stretches and weaken until they no longer provide enough support for the uterus to stay in place. As a result, the uterus slips down into the vagina or protrudes out of the vagina.
Uterine prolapse most often affects people after menopause who’ve had one or more vaginal deliveries.
Mild uterine prolapse usually doesn’t require treatment. But uterine prolapse that causes discomfort or disrupts daily life might benefit from treatment
-
Symptoms
Mild uterine prolapse is common after childbirth. It generally doesn’t cause symptoms. Symptoms of moderate to severe uterine prolapse include:
Seeing or feeling tissue bulge out of the vagina — patient’s usually complaint of mass per vagina.
Feeling heaviness or pulling in the pelvis
Feeling like the bladder doesn’t empty all the way when you use the bathroom
Problems with leaking urine, also called incontinence
Trouble having a bowel movement and needing to press the vagina with your fingers to help have a bowel movement
Feeling as if you have vaginal tissue rubbing on undergarments
Pressure or discomfort in the pelvis or low back
Sexual concerns, such as feeling as though the vaginal tissue is loose
-
Causes
Uterine prolapse results from the weakening of pelvic muscles and supportive tissues. Causes of weakened pelvic muscles and tissues include:
Vaginal delivery
Age at first delivery (older women are at higher risk of pelvic floor injuries compared with younger women)
Difficult labor and delivery or trauma during childbirth
Delivery of a large baby
Being overweight
Lower estrogen level after menopause
Chronic constipation or straining with bowel movements
Chronic cough or bronchitis
Repeated heavy lifting
-
Risk factors
Factors that can increase the risk of uterine prolapse include:
Having one or more vaginal births
Giving birth to a large baby
Aging
Obesity
Prior pelvic surgery
Chronic constipation or often straining during bowel movements
Family history of weak connective tissue
Being Hispanic or white
Chronic coughing, such as from smoking
-
Complications
Uterine prolapse often happens with prolapse of other pelvic organs. These types of prolapse can also happen:
Anterior prolapse. Anterior prolapse results from weak connective tissue between the bladder and roof of the vagina. It can cause the bladder to bulge into the vagina. This is called a cystocele or prolapsed bladder.
Posterior vaginal prolapse. Weak connective tissue between the rectum and the floor of the vagina can cause the rectum to bulge into the vagina. This might cause difficulty with bowel movements. Posterior vaginal prolapse is also called a rectocele.
-
Prevention
To reduce the risk of uterine prolapse, try to:
Prevent constipation. Drink plenty of fluids and eat high-fiber foods, such as fruits, vegetables, beans and whole-grains, brown rice, emperor’s rice.
Avoid heavy lifting. If you have to lift something heavy, do it correctly. Correct lifting uses the legs instead of the waist or back.
Control coughing. Get treatment for a chronic cough or bronchitis. Don’t smoke.
Avoid weight gain. Talk with your doctor about your ideal weight and get advice on how to lose weight, if you need to.
-
Diagnosis
A diagnosis of uterine prolapse often occurs during a pelvic exam. During the pelvic exam (per speculum) your gynecologist may have you:
Bear down as if having a bowel movement. This can help your gynecologist assess how far the uterus has slipped into the vagina.
Tighten your pelvic muscles as if you’re stopping a stream of urine. This test checks the strength of pelvic muscles.
If you have severe urinary incontinence, you might have tests to measure how well your bladder works. This is called urodynamic testing.
-
Treatment
If you have uterine prolapse and it doesn’t bother you, treatment may not be needed. You might choose to wait and see what happens. But when prolapse symptoms bother you, your gynecologist may suggest:
Self-care measures. Self-care measures might provide relief from symptoms or help prevent the prolapse from getting worse. Self-care measures include performing exercises to strengthen pelvic muscles. These are called Kegel exercises. You might also benefit from losing weight and treating constipation.
A pessary. A vaginal pessary is a silicone device inserted into the vagina. It helps prop up bulging tissues. A pessary must be removed regularly for cleaning. This is only a temoporary measure.
-
Surgery
Surgery may be needed to repair uterine prolapse. Minimally invasive surgery, called Robotic surgery, laparoscopic surgery, or vaginal surgery might be an option. If you only have a uterine prolapse, surgery may involve:
Taking out the uterus. This is called a hysterectomy. Hysterectomy may be recommended for uterine prolapse.
A procedure that keeps the uterus in place. This is called a uterus-sparing procedure. These surgeries are for people who might want to have another pregnancy. There is less information on how effective these types of surgeries are. More study is needed.
But if you have prolapse of other pelvic organs along with uterine prolapse, surgery may be a bit more involved. Along with a hysterectomy to take out the uterus, your surgeon may also:
Use stitches to fix weak pelvic floor structures. This can be done in a way that keeps the depth and width of the vagina intact for sexual function.
Place a piece of mesh to support vaginal tissues. In this procedure, vaginal tissues are suspended from the tail bone using a synthetic mesh material which heals by fibrosis.
All surgeries have minimal risks. Risks of surgery for uterine prolapse include:
Bleeding
Blood clots in the legs
Infection
Injury to other organs including the bladder, ureters or bowel
Prolapse happens again
Urinary incontinence.
Talk with your health care provider about all your treatment options to be sure you understand the risks and benefits of each.